About me
I am a neurologist and researcher of the pathological effects that exaggerated sympathetic responses exert on different body systems. In 2012, after years of scientific and clinical training in neuroscience, immunology, and neurology, I took a recreational freediving course that unexpectedly introduced me to the most powerful neurological reflex I know: the mammalian diving response (MDR). This multi-pronged neurological response to prolonged voluntary and involuntary apnea, provides a unique theoretical framework which matches the pathophysiological effects routinely associated with potentially lethal seizures, and the autopsy findings associated with SUDEP victims.
Blood transiently shifted by the MDR could precipitate SUDEP
Pulmonary edema occurs when the fluid inside pulmonary capillaries leaks into, or through, the capillary-alveolar membrane. This edema hinders, or blocks altogether, gas exchange between alveoli and red blood cells. The end result is low blood oxygen.
Several studies show that convulsive seizures often cause various degrees of transient pulmonary edema. Such edema is probably precipitated by increased blood flow through the pulmonary capillaries. As voluntary and involuntary periods of apnea cause the MDR to induce a rapid shift of blood from the periphery into the pulmonary circulation, it is possible, and likely, that seizure-induced pulmonary edema is driven by episodes of seizure-induced apnea that trigger the MDR.
Can SUDEP be predicted?
At any given time, over 60% of the body’s circulating polymorphonucleocytes (a type of immune cell that includes neutrophils, basophils, eosinophils and MAST cells) are in transit through the lungs. But when pulmonary blood flow increases, as it happens when people exercise , become anxious , or have a convulsive seizure , these immune cells are propelled back into the peripheral blood, causing detectable elevations of the white blood cell count (WBCC). It is therefore possible, and likely, that the blood shift of the MDR, which increases pulmonary blood flow during apnea, explains the transient elevations of the WBCC after seizures. Could these elevations reflect SUDEP risk?
Circulating immune cells can reflect pulmonary blood flow during deadly seizures
Most, if not all , epileptic convulsions result in white blood cell count (WBCC) elevations whose magnitudes correlate with clinical outcomes. In addition, these WBCC elevations appear to mirror the degree of breathing abnormalities experienced during or after epileptic convulsions. Taken together, these observations point to the WBCC after seizures as a reflection of pulmonary blood flow during prolonged periods of apnea (or otherwise ineffective breathing) during seizures.
White blood cell counts after seizures may identify patients at risk of SUDEP
The majority of circulating white blood cells (WBCs) are marginated inside the enormous network of pulmonary capillaries. This is why even minor physiological increases in pulmonary blood flow can expel a portion of these cells into the peripheral circulation and drive transient but detectable increases in the WBC count.
As the MDR appears to be triggered during voluntary or involuntary periods of “dry” apnea, transient elevations in the WBC count after seizures suggest that involuntary apnea occurs during or immediately after those seizures. This video shows why and how the WBC count measured after seizures could help identify patients whose epileptic seizures place them at risk of SUDEP.
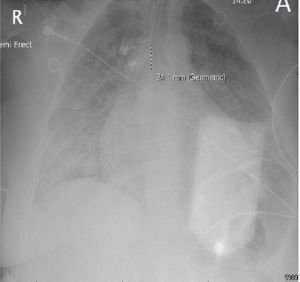
Severe pulmonary edema in a near-SUDEP patient with stereotypical troponin elevations and increased white blood cell counts.
Patients that go into cardiac arrest after a seizure and are successfully resuscitated for at least one hour are said to have experienced a “near SUDEP” event. I had such a patient in 2023. She had suffered intermittent epileptic seizures most of her life but never pursued medical care. Thus, she would have met “probable” SUDEP criteria had she not been resuscitated. The severity of her pulmonary edema and its correlation with transiently increased white blood cell counts suggest that her seizures triggered a surge of systemic catecholamines that likely precipitated her sudden and unexpected demise.
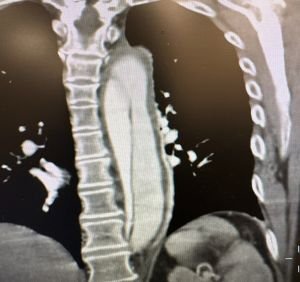
Can seizures cause a non-SUDEP sudden death by provoking hemorrhages inside the walls of large blood vessels?
Sometimes arterial dissection – the pathological splitting of a blood vessel wall by an expanding intramural hemorrhage – hinders blood flow to the brain, or drives the formation of blood clots that cause cerebral infarctions and subsequent epileptic seizures; these seizures are typically said to be symptoms of the arterial dissections. However, some hours usually pass before strokes cause acute symptomatic seizures , raising the question of whether seizures at the onset of arterial dissections are triggers and not symptoms of those dissections.
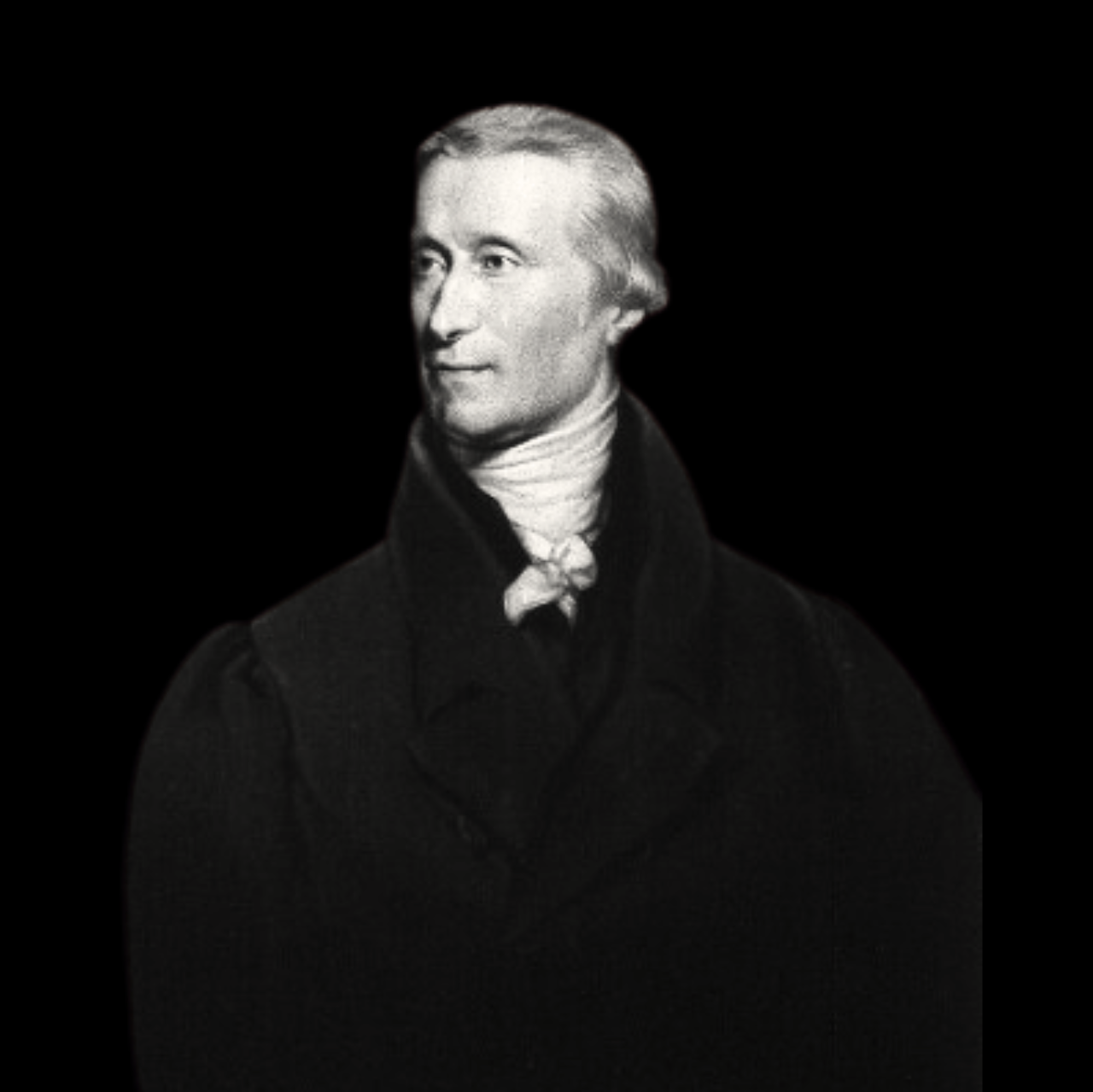
How I came to rewrite the history of the mammalian diving response
The science behind the mammalian diving response originated with the discovery of diving bradycardia, a primordial oxygen-conserving reflex by which the heart rate of air-breathing vertebrates, including humans, slows down in response to prolonged breathing cessation (i.e., apnea). Curiously, luminaries in the field erroneously attributed its discovery to a famous French physician, Paul Bert , even though his experiments were neither intended nor adequate for such a discovery. Instead, diving bradycardia had been described in the doctoral thesis of a medical student (Edmund Goodwyn) almost 100 years before Bert’s work was published. Ironically, his thesis is appropriately referenced in Bert’s own list of citations .